Esophagus High Yield
Page 1 of 1
 Esophagus High Yield
Esophagus High Yield
Mallory-Weiss Tear/syndrome “painless hematemesis”
Pathogenesis: Partial mucosal tear at gastroesophageal junction due to sudden and severe increase in intra-abdominal pressure, usually secondary to retching and/or vomiting.
Classic exam vignette: patient with eating disorder (bulimics, anorexics with self-induced vomiting) or alcoholic who vomits, vomits, vomits, then vomits blood (hematemesis).
Association: hiatal hernia*
Diagnosis: upper endoscopy
Treatment: Usually self-resolving, so the trick answer = No Rx, or just observe with IV fluids and/or blood transfusion. However, if bleeding is persistent, then you proceed to upper endoscopy with vasoconstrictive meds like epinephrine and staunch the bleeding with electrocautery, clips, or thermal coagulation.
How STEP1 can test anatomy: what artery should be embolized to achieve hemostasis of an intractable Mallory-Weiss Tear? Think: what artery perfuses the distal portion of the esophagus? Left Gastric
How to distinguish from variceal bleeding? H/o ESLD (cirrhosis), stigmata: spider nevi, palmar erythema, ascites, etc. Variceal bleeding = venous bleed.
*Quick word about hernia: SLIDING HIATAL hernia is MOST common. Congenital diaphragmatic hernia will cause polyhydramnios. Why? Stomach encroaching upon thoracic cavity --> compresses lung --> pulmonary hypoplasia --> fetus can’t swallow amniotic fluid --> polyhydramnios. On the other hand in Potter Sequence: underdeveloped kidneys --> can’t make urine --> oligohydramnios
Boerhaave Tear/syndrome
Similar principle as Mallory-Weiss. HOWEVER, the tear is TRANSMURAL leading to perforation of esophagus. So rather than painless hematemesis, you have expulsion of air from GI track into the mediastinum, leading to subcutaneous emphysema, crepitus (palpation of patient's chest reveal "crackly air-pockets like popping bubble-wrap", and pneumo-mediastinum. Treatment: this is a surgical emergency
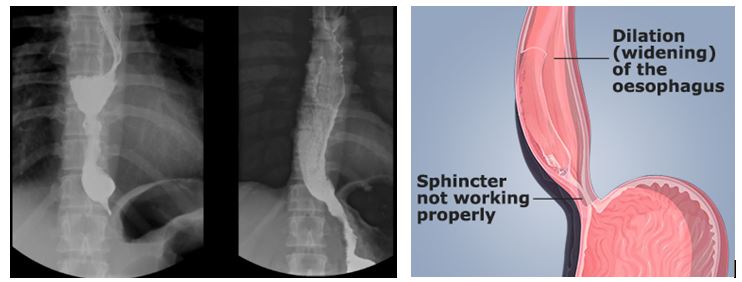
GERD “heartburn”
Pathophysiology: TLESR = transient lower esophageal sphincter relaxation --> reflux of gastric acid up esophagus resulting in heart burn, epigastric pain, dyspepsia, halitosis, cough, hoarseness.
Step 1 Peril:
NOT all that wheezes is asthma. If patient comes in wheezing, dyspneic, wakes up in the middle of the night coughing, but also is: overweight, has reflux symptoms, recent voice changes, chances are it’s the GERD that’s causing the cough, as recumbent position predisposes to reflux that irritates the larynx, voicebox, and oropharynx leading to laryngitis, hoarseness, and chronic cough. Additionally, intraabdominal pressure increases as you go from standing/sitting to reclining position, thereby exacerbating reflux.
Diagnosis: Usually it’s a diagnosis of treatment inclusion. What do you mean? If you suspect GERD, and there’s NO red flags, then empirically treat the GERD with PPI, and if symptoms improve, then it’s most likely GERD.
Step 1 Peril:
What if Patient fails PPI? 1st optimize PPI = confirm BID compliance, increase dose of 1st PPI or switch to another PPI. What if patient still fail? Bring the patient back and order EKG + Cardiac Enzyme to rule out cardiac chest pain, PFT’s to rule out COPD/Asthma and 24Hr pH monitoring for GERD and endoscopy to evaluate for Barrett’s esophagus/esophageal adenocarcinoma. Manometry will reveal ↓LES pressure
What are GERD RED FLAGS? Weight loss, dysphagia, odynophagia, melena, age > 50, anemia, etc.
Step 1 Peril:
Why do pregnancy, diabetes, and systemic sclerosis worsen reflux? “Delayed- Gastric Emptying” Impaired esophageal motility secondary to effects of progesterone, diabetic ischemic neuropathy/gastroparesis, excess collagen deposition in esophageal smooth muscle. How do you treat GERD in pregnancy? 1st lifestyle modification 2nd Calcium antacid.
GERD 1st line Treatment: Lifestyle modification. If that fails, then 2nd line go straight for PPI like omeprazole, proven to be superior to H2 blockers. If there’s a concomitant hernia that's contributing to GERD, then do surgery: NISSEN fundoplication.
What are the GERD lifestyle modifications? Elevate head of bed, limit hot, spicy, fatty foods, eat smaller portion, stop drinking and stop smoking, exercise.
GERD Complication 1. Barrett’s Esophagus and Esophageal Adenocarcinoma
GERD Complication 2. Esophageal stricture*
*Esophageal squamous cells deal with acid in 2 ways: either undergo metaplastic transformation into more “stomach” like columnar cells or form scar (collagen deposition) = luminal narrowing stricture. Thus, patient with long-standing GERD might complain of progressive dysphagia to solid foods.
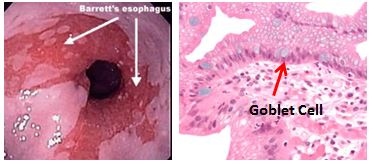
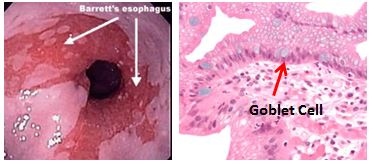
Barrett’s esophagus
Pathophysiology: Metaplasia of esophagus. Essentially, the esophagus with its mucosal coating of stratified squamous epithelium is not equipped to deal with acid very well. However, these squamous cells contain stem cells that can undergo METAPLASIA into goblet containing columnar cells, which handles acid fairly well. Nonetheless, unbridled metaplasia can invite dysplasia and eventually carcinogenesis, leading to esophageal ADENOCARCINOMA.
What are the main risk factors? Chronic reflux aka GERD no.1, esophagitis, ulcers, obesity
So how is this any different than GERD? They both present with similar, if almost identical signs and symptoms. Only direct endoscopy with biopsy will differentiate.
Treatment is similar to GERD: 1st line lifestyle modification 2nd line PPI, regular endoscopic surveillance
Esophagus Cancer
The two main types you have to know are Esophageal Adenocarcinoma, Adeno = “glandular”
which usually arises in setting of chronic GERD/Barrett’s esophagus and Esophageal Squamous Cell Carcinoma, which arises in setting of chronic irritation: 2 most important risk factors in Esophageal SCC = SMOKING & ALCOHOL. Other risks: hot or spicy foods, Zenker Diverticula, Esophageal web
Classic Exam vignette: Patient complains of progressive dysphagia first to solids then to liquids and WEIGHT LOSS. Other RED FLAGS: odynophagia, melena, hematemesis, old age, etc.
What does STEP1 like to test? Like pancreatic adenocarcinoma & gastric adenocarcinoma, esophageal adenocarcinoma can present with supraclavicular lymphadenopathy “Virchow’s node”. Esophageal SCC can cause hypercalcemia via secretion of PTHrP (paraneoplastic syndrome).
Dysphagia
How does dysphagia help you narrow down disease?
Progressive Dysphagia: first to solids then liquids, which reflects NARROWING or OBSTRUCTION of the esophageal lumen. What narrows or obstructs? Cancer, Stricture, Achalasia (narrowed LES)
Dysphagia to Solids and Liquids at the same time, which reflects intrinsic dysmotility of the esophageal smooth muscle. What affects peristalsis? Diabetes, Systemic Sclerosis, Infiltrative disease like amyloid, sarcoid, hemochromatosis etc. How does diabetes cause this? Ischemia to vagal efferent nerves innervating esophageal smooth muscle resulting in “gastroparesis” = GI weakness. How does systemic sclerosis or amyloidosis or hemochromatosis cause this? Excess deposition of collagen, or amyloid protein, or hemosiderin in the esophagus smooth muscle impair normal motility
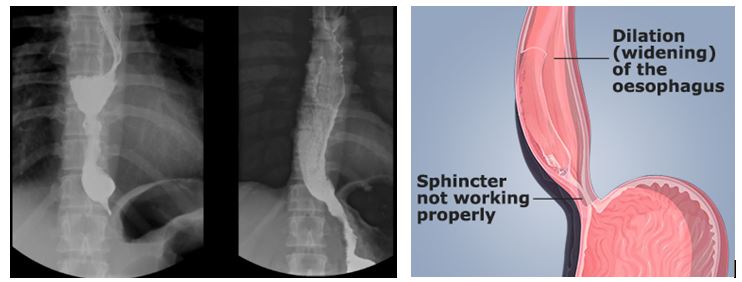
Achalasia “a-chalasis” aka “no-relaxation”
Pathophysiology: no.1 most common distal esophagus motor disorder. Autoimmune triggered loss of ENS myenteric (Auerbach) plexus & NO-secreting neurons result in impaired relaxation of lower esophageal sphincter (LES).
STEP1 Peril:
What is the embryologic derivative of these abnormally migrant neurons? neural crest cells
What does manometry show? High LES resting pressure and diffuse “esophageal spasm”.
Why kind of dysphagia? Initially progressive (solids --> liquids). Later as esophageal motility is deranged, you get dysphagia to both solids and liquids simultaneously.
What does barium swallow show? “Bird’s beak”
What type of esophageal cancer is achalasia at increased risk for? Esophageal SCC
Why MUST you always order upper endoscopy? If you suspect achalasia, you MUST scope patient to rule out esophageal cancer masquerading as pseudo-achalasia, which can mimic the progressive dysphagia symptom.
Secondary achalasia can arise from what parasitic infection? Chagas disease T. cruzi amastigotes destroy ganglion cells = must treat with Nifurtomox or Benznidazole
How do you treat achalasia? Medically relax LES via CCB (nifedipine*) or nitrates or botox. Surgically myotomy or balloon dilation of LES.
*Review non-dihydropyridine calcium channel blocker are great for treating and as prophylaxis for “spasm” diseases like 1) post sub-arachnoid hemorrhage cerebral vascular spasm 2) Raynaud’s digital vasospasm 3) achalasia esophageal spasm 4) Prinzmetal variant angina coronary spasm
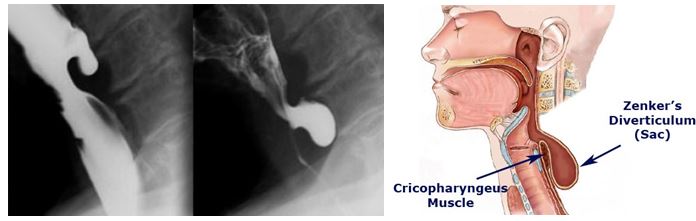
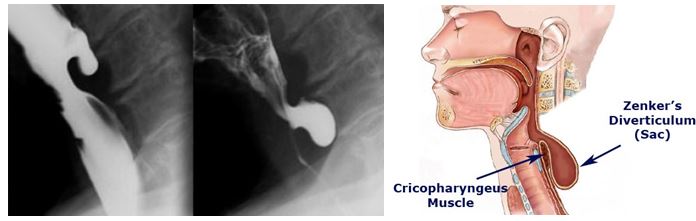
Zenker Diverticulum
Pathophysiology: false diverticula involving only mucosa through upper esophagus due to weakness in the cricopharyngeus muscle.
Classic Exam vignette: elderly patient complains of dysphagia, choking on food, halitosis, and regurgitating undigested food. Palpation of neck might reveal “fluctuant mass”
Complications: Aspiration pneumonia
Diagnosis: Barium Swallow. AVOID upper endoscopy as this can cause iatrogenic perforation
Treatment: surgical myotomy of cricopharyngeal muscle
Step 1 Anatomy Peril: What nerve innervates cricopharyngeus? Most all pharyngeal constrictors are innervated by Vagus nerve.
Pathogenesis: Partial mucosal tear at gastroesophageal junction due to sudden and severe increase in intra-abdominal pressure, usually secondary to retching and/or vomiting.
Classic exam vignette: patient with eating disorder (bulimics, anorexics with self-induced vomiting) or alcoholic who vomits, vomits, vomits, then vomits blood (hematemesis).
Association: hiatal hernia*
Diagnosis: upper endoscopy
Treatment: Usually self-resolving, so the trick answer = No Rx, or just observe with IV fluids and/or blood transfusion. However, if bleeding is persistent, then you proceed to upper endoscopy with vasoconstrictive meds like epinephrine and staunch the bleeding with electrocautery, clips, or thermal coagulation.
How STEP1 can test anatomy: what artery should be embolized to achieve hemostasis of an intractable Mallory-Weiss Tear? Think: what artery perfuses the distal portion of the esophagus? Left Gastric
How to distinguish from variceal bleeding? H/o ESLD (cirrhosis), stigmata: spider nevi, palmar erythema, ascites, etc. Variceal bleeding = venous bleed.
*Quick word about hernia: SLIDING HIATAL hernia is MOST common. Congenital diaphragmatic hernia will cause polyhydramnios. Why? Stomach encroaching upon thoracic cavity --> compresses lung --> pulmonary hypoplasia --> fetus can’t swallow amniotic fluid --> polyhydramnios. On the other hand in Potter Sequence: underdeveloped kidneys --> can’t make urine --> oligohydramnios
Boerhaave Tear/syndrome
Similar principle as Mallory-Weiss. HOWEVER, the tear is TRANSMURAL leading to perforation of esophagus. So rather than painless hematemesis, you have expulsion of air from GI track into the mediastinum, leading to subcutaneous emphysema, crepitus (palpation of patient's chest reveal "crackly air-pockets like popping bubble-wrap", and pneumo-mediastinum. Treatment: this is a surgical emergency
GERD “heartburn”
Pathophysiology: TLESR = transient lower esophageal sphincter relaxation --> reflux of gastric acid up esophagus resulting in heart burn, epigastric pain, dyspepsia, halitosis, cough, hoarseness.
Step 1 Peril:
NOT all that wheezes is asthma. If patient comes in wheezing, dyspneic, wakes up in the middle of the night coughing, but also is: overweight, has reflux symptoms, recent voice changes, chances are it’s the GERD that’s causing the cough, as recumbent position predisposes to reflux that irritates the larynx, voicebox, and oropharynx leading to laryngitis, hoarseness, and chronic cough. Additionally, intraabdominal pressure increases as you go from standing/sitting to reclining position, thereby exacerbating reflux.
Diagnosis: Usually it’s a diagnosis of treatment inclusion. What do you mean? If you suspect GERD, and there’s NO red flags, then empirically treat the GERD with PPI, and if symptoms improve, then it’s most likely GERD.
Step 1 Peril:
What if Patient fails PPI? 1st optimize PPI = confirm BID compliance, increase dose of 1st PPI or switch to another PPI. What if patient still fail? Bring the patient back and order EKG + Cardiac Enzyme to rule out cardiac chest pain, PFT’s to rule out COPD/Asthma and 24Hr pH monitoring for GERD and endoscopy to evaluate for Barrett’s esophagus/esophageal adenocarcinoma. Manometry will reveal ↓LES pressure
What are GERD RED FLAGS? Weight loss, dysphagia, odynophagia, melena, age > 50, anemia, etc.
Step 1 Peril:
Why do pregnancy, diabetes, and systemic sclerosis worsen reflux? “Delayed- Gastric Emptying” Impaired esophageal motility secondary to effects of progesterone, diabetic ischemic neuropathy/gastroparesis, excess collagen deposition in esophageal smooth muscle. How do you treat GERD in pregnancy? 1st lifestyle modification 2nd Calcium antacid.
GERD 1st line Treatment: Lifestyle modification. If that fails, then 2nd line go straight for PPI like omeprazole, proven to be superior to H2 blockers. If there’s a concomitant hernia that's contributing to GERD, then do surgery: NISSEN fundoplication.
What are the GERD lifestyle modifications? Elevate head of bed, limit hot, spicy, fatty foods, eat smaller portion, stop drinking and stop smoking, exercise.
GERD Complication 1. Barrett’s Esophagus and Esophageal Adenocarcinoma
GERD Complication 2. Esophageal stricture*
*Esophageal squamous cells deal with acid in 2 ways: either undergo metaplastic transformation into more “stomach” like columnar cells or form scar (collagen deposition) = luminal narrowing stricture. Thus, patient with long-standing GERD might complain of progressive dysphagia to solid foods.
Barrett’s esophagus
Pathophysiology: Metaplasia of esophagus. Essentially, the esophagus with its mucosal coating of stratified squamous epithelium is not equipped to deal with acid very well. However, these squamous cells contain stem cells that can undergo METAPLASIA into goblet containing columnar cells, which handles acid fairly well. Nonetheless, unbridled metaplasia can invite dysplasia and eventually carcinogenesis, leading to esophageal ADENOCARCINOMA.
What are the main risk factors? Chronic reflux aka GERD no.1, esophagitis, ulcers, obesity
So how is this any different than GERD? They both present with similar, if almost identical signs and symptoms. Only direct endoscopy with biopsy will differentiate.
Treatment is similar to GERD: 1st line lifestyle modification 2nd line PPI, regular endoscopic surveillance
Esophagus Cancer
The two main types you have to know are Esophageal Adenocarcinoma, Adeno = “glandular”
which usually arises in setting of chronic GERD/Barrett’s esophagus and Esophageal Squamous Cell Carcinoma, which arises in setting of chronic irritation: 2 most important risk factors in Esophageal SCC = SMOKING & ALCOHOL. Other risks: hot or spicy foods, Zenker Diverticula, Esophageal web
Classic Exam vignette: Patient complains of progressive dysphagia first to solids then to liquids and WEIGHT LOSS. Other RED FLAGS: odynophagia, melena, hematemesis, old age, etc.
What does STEP1 like to test? Like pancreatic adenocarcinoma & gastric adenocarcinoma, esophageal adenocarcinoma can present with supraclavicular lymphadenopathy “Virchow’s node”. Esophageal SCC can cause hypercalcemia via secretion of PTHrP (paraneoplastic syndrome).
Dysphagia
How does dysphagia help you narrow down disease?
Progressive Dysphagia: first to solids then liquids, which reflects NARROWING or OBSTRUCTION of the esophageal lumen. What narrows or obstructs? Cancer, Stricture, Achalasia (narrowed LES)
Dysphagia to Solids and Liquids at the same time, which reflects intrinsic dysmotility of the esophageal smooth muscle. What affects peristalsis? Diabetes, Systemic Sclerosis, Infiltrative disease like amyloid, sarcoid, hemochromatosis etc. How does diabetes cause this? Ischemia to vagal efferent nerves innervating esophageal smooth muscle resulting in “gastroparesis” = GI weakness. How does systemic sclerosis or amyloidosis or hemochromatosis cause this? Excess deposition of collagen, or amyloid protein, or hemosiderin in the esophagus smooth muscle impair normal motility
Achalasia “a-chalasis” aka “no-relaxation”
Pathophysiology: no.1 most common distal esophagus motor disorder. Autoimmune triggered loss of ENS myenteric (Auerbach) plexus & NO-secreting neurons result in impaired relaxation of lower esophageal sphincter (LES).
STEP1 Peril:
What is the embryologic derivative of these abnormally migrant neurons? neural crest cells
What does manometry show? High LES resting pressure and diffuse “esophageal spasm”.
Why kind of dysphagia? Initially progressive (solids --> liquids). Later as esophageal motility is deranged, you get dysphagia to both solids and liquids simultaneously.
What does barium swallow show? “Bird’s beak”
What type of esophageal cancer is achalasia at increased risk for? Esophageal SCC
Why MUST you always order upper endoscopy? If you suspect achalasia, you MUST scope patient to rule out esophageal cancer masquerading as pseudo-achalasia, which can mimic the progressive dysphagia symptom.
Secondary achalasia can arise from what parasitic infection? Chagas disease T. cruzi amastigotes destroy ganglion cells = must treat with Nifurtomox or Benznidazole
How do you treat achalasia? Medically relax LES via CCB (nifedipine*) or nitrates or botox. Surgically myotomy or balloon dilation of LES.
*Review non-dihydropyridine calcium channel blocker are great for treating and as prophylaxis for “spasm” diseases like 1) post sub-arachnoid hemorrhage cerebral vascular spasm 2) Raynaud’s digital vasospasm 3) achalasia esophageal spasm 4) Prinzmetal variant angina coronary spasm
Zenker Diverticulum
Pathophysiology: false diverticula involving only mucosa through upper esophagus due to weakness in the cricopharyngeus muscle.
Classic Exam vignette: elderly patient complains of dysphagia, choking on food, halitosis, and regurgitating undigested food. Palpation of neck might reveal “fluctuant mass”
Complications: Aspiration pneumonia
Diagnosis: Barium Swallow. AVOID upper endoscopy as this can cause iatrogenic perforation
Treatment: surgical myotomy of cricopharyngeal muscle
Step 1 Anatomy Peril: What nerve innervates cricopharyngeus? Most all pharyngeal constrictors are innervated by Vagus nerve.
Page 1 of 1
Permissions in this forum:
You cannot reply to topics in this forum