Cirrhosis High Yield
Page 1 of 1
 Cirrhosis High Yield
Cirrhosis High Yield
Cirrhosis
What is it? It is irreversible nodular sclerosis of liver. Again, it is IRREVERSIBLE.
What is no.1 cause in US? Chronic Alcohol
What is no.1 infection cause? HCV (more common chronic hepatitis than HBV, which is more commonly associated with HCC)
So what does irreversible mean? If patient stops drinking for 3 years, their cirrhotic liver is STILL cirrhotic. If they completely cure their HCV infection with Harvoni (Sofosbuvir/ledipasvir), their cirrhotic liver is STILL cirrhotic. However, if their liver were fibrotic instead of cirrhotic, then cessation of alcohol or HCV clearance can induce reversal of fibrosis, which unlike cirrhosis, is reversible.
So what happens to cirrhotic liver? I like to think of it as, what can a failed liver NOT do for you?
1. Synthesis: Coagulation factors
Remember, liver has VitK Epoxide Reductase which gamma-carboxylates Factors II, VII, IX, X, Protein C & S, attaching anionic carboxyl groups to these factors making them more "sticky" to the cationic phospholipid surface of platelets. So a F'd up liver can't activate these coagulation factors, so your PT and PTT times increase. Generally, doctors measure PT first, because it's an earlier marker of liver failure. PTT will increase too, albeit, later
STEP1 Peril: why are you also more prone to bleeding (increase bleeding time)? Cirrhosis causes portal HTN which causes backup of blow flow across splenic vein into the sinusoids of the spleen, causing splenomegaly and squestration of platelets, leading to thrombocytopenia.
STEP1 Peril: What's the treatment for cirrhosis bleeding, i.e. a patient with cirrhosis comes in to get blood drawn, but then bleeds profusely from venipuncture sites? Fresh Frozen Plasma ***
FFP on STEP1 is used for A) Liver Failure acute bleeding B) Warfarin reversal acute bleeding C) DIC acute bleeding. Why not VitK? It takes several days for VitK to be used as a coenzyme by hepatocyte epoxide reductase and is NOT indicated in the emergent situation. Why not cryoprecipitate? It too has many coagulation factors as FFP, however, the general rule of thumb for STEP1 is to go with the MOST COMMON answer. FFP is more commonly used than cryoprecipitate, which also is very cumbersome to defrost and make readily available.
2. Synthesis: Albumin
Albumin on STEP1 carries A)Triglyceride/cholesterol B)unconjugated bilirubin C) Vitamins D) ions like Ca2+ and ACTS as the MOST important Oncotic solute, thereby contributing to intravascular oncotic pressure. It "Pulls" extravasated fluid back into vessel lumen. Without Albumin you can get additional fluid leaking out = ascites ***
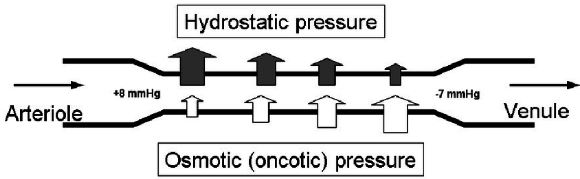
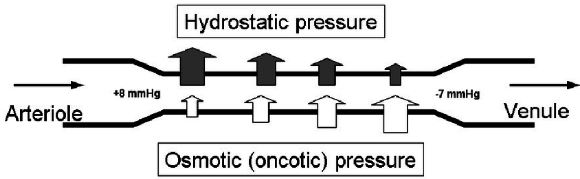
***What two factors contribute to ascite formation in Cirrhosis? Remember Starling Forces?
1) Portal HTN --> increased hydrostatic pressure within splanchnic circulation aka superior and inferior mesenteric venous plexi
2) Failing liver can't make adequate albumin --> decreased oncotic pressure.
Since we're on the topic of Ascites, why don't we talk about it more.
What is no.1 cause of ascites? Cirrhosis. No.1 cause of cirrhosis? Chronic alcoholism
What da heck is SAAG? It's a math equation that helps evaluate the cause of ascites.
SAAG = Serum Albumin - Ascites Albumin. This Gradient should normally be 0, because the albumin content in serum and ascites are fairly identical. What happens in cirrhosis portal hypertension? In cirrhosis, yes, the albumin level is decreased throughout the body because the liver is not making it adequately. However, this decrease is NOT evenly distributed across body lumens and cavities. Why not?? The high hydrostatic pressure from portal hypertension forces a lot of water out of the vessel into the peritoneal cavity (peritoneum), thereby "diluting" the albumin concentration on the "ascites" side, or the peritoneum. Thus the SAAG >1.1 indicates ascites due to portal hypertension.
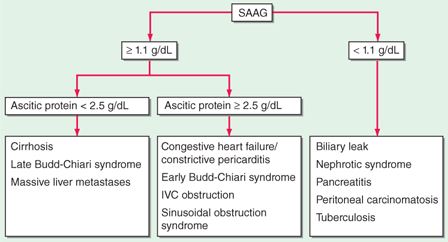
Don't worry about this busy flowchart too much. Anytime STEP1 labs have Ascites albumin and Serum albumin and SAAG >1.1 you know it involves diseases of increased hydrostatic pressure 1) cirrhosis portal HTN 2) budd-chiari hepatic vein thrombosis HTN 3) CHF systemic HTN etc.
So how do you treat Ascites? Similarly to excess fluid accumulation in CHF, STEP1 and medical teaching follows these rules
1. 1st Line Lifestyle modification: stop drinking, stop smoking, go easy on the salt and pepper
2. If lifestyle modifcation fails: water pill, i.e. furosemide (Lasix) or aldosterone antagonist: spironolactone (prevents Na retention) or Eplerenone (if patient also has concomittant gynecomastia secondary to impaired steroid metabolism by failing liver, resulting in increased circulating estrogen)
3. If lifestyle modifcation + water pill fail, then you have to "poke" the patient = therapeutic paracentesis. Patients with severe cirrhosis ascites not uncommonly go to their liver doctor for weekly needle pokes to draw out 1-2 liters of fluid from their peritoneum.
***Note, the above paradigm applies to "frequent flyer" patients, meaning, you know they have cirrhosis ascites and have seen them multiple times. If, however, a NEW patient first comes to you with belly full of fluid, you MUST also "poke" them first to rule out bacterial peritonitis with a diagnostic paracentesis.
STEP1 Peril:
What is drawing fluid from joint? Arthrocentesis, to diagnose and treat septic arthritis and gout
What is drawing fluid or air from pleural cavity? Thoracocentesis to diagnose and treat pneumothorax, parapneumonic effusion, empyema via Light's Criteria
What is drawing fluid or air from pericardial cavity? Pericardiocentesis to diagnose and treat pericardial tampondate (hemopericardium), or infiltrative disease like HH, amyloidosis, or cancer that cause fluid in the pericardial sac
Spontaneous Bacterial Peritonitis (SBP). This is when ascites fluid becomes infected with gut bacteria (usually GNR like E. coli and/or anaerobes).
How does someone with peritonitis present? INTENSE abdominal pain and ...
"Guarding" why? They tense their abdominal muscles to "protect" their peritoneum from further motion and irritation. You feel vague abdominal pain from your VISCERAL pain fibers on the visceral peritoneum.
"Rebound tenderness" why? Again, sudden removal of the examiner's fingers cause a precipitous reverberating motion on the peritoneum which causes frictional irritation to the visceral peritoneal pain fibers.
How does someone with peritonitis AND ascites present? No or very minimal Abdominal pain. Why? The ascites fluid acts like a "water balloon" cushioning the parietal peritoneum and the visceral peritoneum, thereby minimizing the frictional irritation from provocative physical exam maneuvers. This is important, because ascites patients can have peritonitis despite NO abdominal symptoms other than a low grade fever.
So what is the STEP1 criteria for SBP? Paracentesis ASCITES FLUID PMN > 250, or a Positive Culture . Of course, you must also send it for total cell count, glucose, albumin,etc. You might get an oddball question about "milky" fluid in ascites. ANYTIME you have "milky" or "thick white" fluid in a CAVITY think Chylous or lymphatic rupture = triglycerides and/or lymphoma
What about bloody fluid? TB, TB, TB or CANCER, CANCER, CANCER
Thus, when should you perform a paracentesis in patients with ascites?
1) ALL first-time patients as diagnostic paracentesis to rule out SBP
2) ALL patients with new onset fever, leukocytosis, bandemia, left shift as diagnostic paracentesis for SBP
3) ALL patients who failed lifestyle modification + medical management as therapeutic paracentesis
3. Breaks stuff down: Ammonia (NH3) via AST/ALT into urea cycle.
So in cirrhosis, you have NH3 build-up leading to hepatic encephalopathy, which basically means A) "neurologically wasted", or everything slows down for patient B) asterixis "hand flapping" when elbows and wrists hyperextended. Exact mechanism has not been elucidated but for STEP1, know that
NH3 potentiates inhibitory neurons, aka GABAergic chloride channels = inhibition = slowing down.
NH3 inhibits excitatory neurons, aka Glutamatergic NMDA channels = inhibition = slowding down.
How do you treat this? Lactulose. Why in the world do you give an undigested sugar to treat hepatic encephalopathy? Because this is ingenious.
Basically, lactulose is like cellulose. Yes, it's NOT digested by our brush border enzymes and therefore reaches the colon intact. There, colonic gut bacteria ferment this sugar as well as All other undigested/unabsorbed sugars into Short Chain Fatty Acids (SCFA). And what do fatty acids have in common? Carboxylic Acid moiety which acidifies the colonic lumen. This then acidifies and ionizes NH3 (ammonia) into +NH4 (ammonium), thereby trapping the polar ionic ammonium within the gut lumen.
In summary,
A. lactulose indirectly acidifies and traps ammonia as polar less absorbable ammonium within the colon lumen for excretion.
B. Lactulose is 1st line treatment.
C. Rifaximin is 2nd line treatment. It is an antibiotic that targets NH3 (ammonia) producing colonic bacteria.
4. Breaks Stuff Down: toxins Hepatopulmonary syndrome
The exact mehanism is not fully understood, but in cirrhosis, a failing liver can't metabolize certain body toxins, some of which target pulmonary vasculature and cause a Nitric-Oxide mediated "global" pulmonary vasodilation. Why is this bad? When you dilate nearly ALL of your pulmonary vasculature, you worsen the physiologic Ventilation-Perfusion mismatch. Why? At rest, Not all of your alveoli and pulmonary vessels are open, but they matched up according to effects of gravity. (see diagram below). When you lie down, this gravity mediated V/Q mismatch is diminished.
Thus in hepatopulmonary syndrome, patients complain of dyspnea standing or sitting, which alleviates with lying down. A fancier term is called platypnea. Contrast this with orthopnea or dyspnea lying down in patients with heart failure, in which lying down causes more venous return to the heart, worsening pulmonary edema, which alleviates with sleeping at an angle. Hence the multiple pillows at night or in some severe CHF patients, they say, "doc, I've been sleeping on a recliner lately".
So STEP1 take-home for HPS: Worsening V-Q mismatch and increased A-a gradient secondary to NO-mediated vasodilation of pulmonary vasculature. This effect is WORSE standing up due to gravity, and gets better lying down = platypnea (dyspnea standing up, better in recumbent position). The only real treatment is? Get a new Liver = transplant.

5. Breaks stuff down: Hepatorenal syndrome
Same concept as hepatopulmonary syndrome. Diseased liver can't metabolize toxins, some of which target renal vasculature and instead of dilation, causes "global" renal vasoconstriction. Other factors include systemic vasodilation which triggers RAAS, ATIII and renal vasoconstriction. But bottom line:This puts kidneys in a chronic perfusion "starved" state and subsequent renal failure. So shitty GFR, Cr clearance, rising BUN:Cr ratio, etc. However, what defines hepatorenal syndrome is FAILURE of aggressive resuscitative fluids to recover renal function. Again, unlike normal acute kideny injury, whereby aggresive fluid administration can reverse the shitty GFR, Cr Clearance, these renal function labs do NOT recover when you give fluids in a patient with HRS. As in HPS, HRS can only be resolved with resolution of the failed liver = transplantation.
6. Abnormal blood flow
In a diseased liver, the splanchnic circulation (i.e. celiac, superior and inferior mesenteric venous plexi) DILATES and "sucks" all the blood from systemic circulation, thereby decreasing effective circulating intravascular volume. Thus a treatment principle hinges on reducing additional splanchnic vasodilation by giving a vasoconstrictor via
1) Non-selective beta-blocker: propranolol. Why non-selective? It does NOT selective for B1. So it's Both B1 and B2 antagonist. ***remember for STEP1 heart contractility, heart rate, conduction velocity = B1. Lungs, gut, uterus smooth muscle relaxation = B2. So bronchodilation = B2. Gut splanchnic vasodilation = B2. Uterus smooth muscle relaxation = B2. Thus, by blocking B2, you impede some of the unwanted splanchnic vasodilation and minimize further blood pooling into the gut, thereby improving the portal HTN. A side-effect, however with Non-selective beta blockers, is as you guessed it, bronchospasm.
2) Octreotide (somatostatin analog), similar principle as non-selective beta-blocker. It causes splanchnic vasoconstriction.
So how do you treat acute esophageal variceal bleed and achieve maintenance prophylaxis against future episodes?
Acute: Octreotide (medical) + sclerotherapy/electrocautery/balloon tamponade (surgical)
Prophylaxis: propranolol
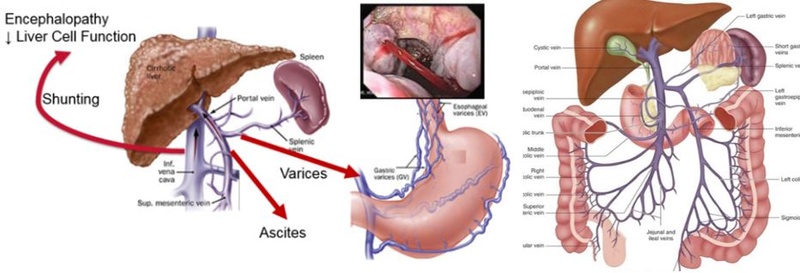
Portal System: Remember mainly all of your "Gut" organs drain first into your liver via the portal system: splenic vein, superior mesenteric vein, and inferior mesenteric vein.
You can get Portal Hypertension by any of the following methods
1) Within the liver: most commonly cirrhosis, less commonly: fibrosis, liver cancer, et.c
2) Outside the liver: portal vein thrombosis
3) Oustide the liver: Hepatic vein thrombosis (Budd-Chiari syndrome)
4) Outside the liver: Right heart failure which is most commonly caused by LHF --> RHF or Constrictive Cardiomyopathy, or anything that evenutally backs up to the right side of the heart and subsequently the liver. This causes a "nutmeg liver"
What happens in portal HTN? The dilated portal veins create new connections "anastamosis" with systemic system as a detour. Otherwise, the vein will keep on dilating and eventually burst.
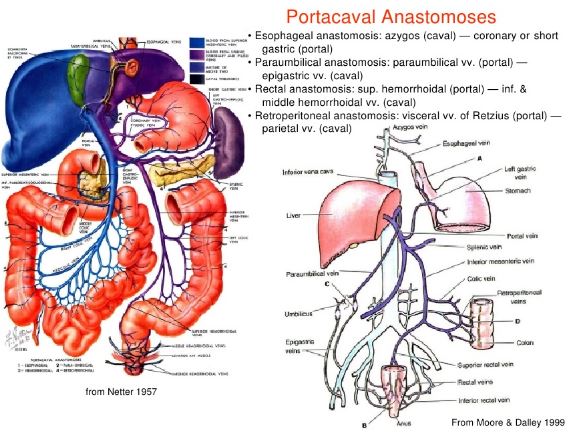
The STEP1 Take-home for Portal-Systemic Anastamosis are:
1. Esophageal: left gastric (portal) to esophageal vein (systemic)
2. Paraumbilical: paraumbilical vein (portal) to epigastric vein (systemic)
3. Rectal: superior hemorrhoidal/rectal vein to middle and inferior hemorrhoidal/rectal vein
What is it? It is irreversible nodular sclerosis of liver. Again, it is IRREVERSIBLE.
What is no.1 cause in US? Chronic Alcohol
What is no.1 infection cause? HCV (more common chronic hepatitis than HBV, which is more commonly associated with HCC)
So what does irreversible mean? If patient stops drinking for 3 years, their cirrhotic liver is STILL cirrhotic. If they completely cure their HCV infection with Harvoni (Sofosbuvir/ledipasvir), their cirrhotic liver is STILL cirrhotic. However, if their liver were fibrotic instead of cirrhotic, then cessation of alcohol or HCV clearance can induce reversal of fibrosis, which unlike cirrhosis, is reversible.
So what happens to cirrhotic liver? I like to think of it as, what can a failed liver NOT do for you?
1. Synthesis: Coagulation factors
Remember, liver has VitK Epoxide Reductase which gamma-carboxylates Factors II, VII, IX, X, Protein C & S, attaching anionic carboxyl groups to these factors making them more "sticky" to the cationic phospholipid surface of platelets. So a F'd up liver can't activate these coagulation factors, so your PT and PTT times increase. Generally, doctors measure PT first, because it's an earlier marker of liver failure. PTT will increase too, albeit, later
STEP1 Peril: why are you also more prone to bleeding (increase bleeding time)? Cirrhosis causes portal HTN which causes backup of blow flow across splenic vein into the sinusoids of the spleen, causing splenomegaly and squestration of platelets, leading to thrombocytopenia.
STEP1 Peril: What's the treatment for cirrhosis bleeding, i.e. a patient with cirrhosis comes in to get blood drawn, but then bleeds profusely from venipuncture sites? Fresh Frozen Plasma ***
FFP on STEP1 is used for A) Liver Failure acute bleeding B) Warfarin reversal acute bleeding C) DIC acute bleeding. Why not VitK? It takes several days for VitK to be used as a coenzyme by hepatocyte epoxide reductase and is NOT indicated in the emergent situation. Why not cryoprecipitate? It too has many coagulation factors as FFP, however, the general rule of thumb for STEP1 is to go with the MOST COMMON answer. FFP is more commonly used than cryoprecipitate, which also is very cumbersome to defrost and make readily available.
2. Synthesis: Albumin
Albumin on STEP1 carries A)Triglyceride/cholesterol B)unconjugated bilirubin C) Vitamins D) ions like Ca2+ and ACTS as the MOST important Oncotic solute, thereby contributing to intravascular oncotic pressure. It "Pulls" extravasated fluid back into vessel lumen. Without Albumin you can get additional fluid leaking out = ascites ***
***What two factors contribute to ascite formation in Cirrhosis? Remember Starling Forces?
1) Portal HTN --> increased hydrostatic pressure within splanchnic circulation aka superior and inferior mesenteric venous plexi
2) Failing liver can't make adequate albumin --> decreased oncotic pressure.
Since we're on the topic of Ascites, why don't we talk about it more.
What is no.1 cause of ascites? Cirrhosis. No.1 cause of cirrhosis? Chronic alcoholism
What da heck is SAAG? It's a math equation that helps evaluate the cause of ascites.
SAAG = Serum Albumin - Ascites Albumin. This Gradient should normally be 0, because the albumin content in serum and ascites are fairly identical. What happens in cirrhosis portal hypertension? In cirrhosis, yes, the albumin level is decreased throughout the body because the liver is not making it adequately. However, this decrease is NOT evenly distributed across body lumens and cavities. Why not?? The high hydrostatic pressure from portal hypertension forces a lot of water out of the vessel into the peritoneal cavity (peritoneum), thereby "diluting" the albumin concentration on the "ascites" side, or the peritoneum. Thus the SAAG >1.1 indicates ascites due to portal hypertension.
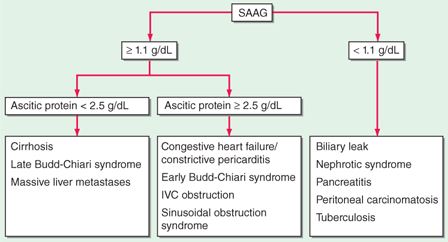
Don't worry about this busy flowchart too much. Anytime STEP1 labs have Ascites albumin and Serum albumin and SAAG >1.1 you know it involves diseases of increased hydrostatic pressure 1) cirrhosis portal HTN 2) budd-chiari hepatic vein thrombosis HTN 3) CHF systemic HTN etc.
So how do you treat Ascites? Similarly to excess fluid accumulation in CHF, STEP1 and medical teaching follows these rules
1. 1st Line Lifestyle modification: stop drinking, stop smoking, go easy on the salt and pepper
2. If lifestyle modifcation fails: water pill, i.e. furosemide (Lasix) or aldosterone antagonist: spironolactone (prevents Na retention) or Eplerenone (if patient also has concomittant gynecomastia secondary to impaired steroid metabolism by failing liver, resulting in increased circulating estrogen)
3. If lifestyle modifcation + water pill fail, then you have to "poke" the patient = therapeutic paracentesis. Patients with severe cirrhosis ascites not uncommonly go to their liver doctor for weekly needle pokes to draw out 1-2 liters of fluid from their peritoneum.
***Note, the above paradigm applies to "frequent flyer" patients, meaning, you know they have cirrhosis ascites and have seen them multiple times. If, however, a NEW patient first comes to you with belly full of fluid, you MUST also "poke" them first to rule out bacterial peritonitis with a diagnostic paracentesis.
STEP1 Peril:
What is drawing fluid from joint? Arthrocentesis, to diagnose and treat septic arthritis and gout
What is drawing fluid or air from pleural cavity? Thoracocentesis to diagnose and treat pneumothorax, parapneumonic effusion, empyema via Light's Criteria
What is drawing fluid or air from pericardial cavity? Pericardiocentesis to diagnose and treat pericardial tampondate (hemopericardium), or infiltrative disease like HH, amyloidosis, or cancer that cause fluid in the pericardial sac
Spontaneous Bacterial Peritonitis (SBP). This is when ascites fluid becomes infected with gut bacteria (usually GNR like E. coli and/or anaerobes).
How does someone with peritonitis present? INTENSE abdominal pain and ...
"Guarding" why? They tense their abdominal muscles to "protect" their peritoneum from further motion and irritation. You feel vague abdominal pain from your VISCERAL pain fibers on the visceral peritoneum.
"Rebound tenderness" why? Again, sudden removal of the examiner's fingers cause a precipitous reverberating motion on the peritoneum which causes frictional irritation to the visceral peritoneal pain fibers.
How does someone with peritonitis AND ascites present? No or very minimal Abdominal pain. Why? The ascites fluid acts like a "water balloon" cushioning the parietal peritoneum and the visceral peritoneum, thereby minimizing the frictional irritation from provocative physical exam maneuvers. This is important, because ascites patients can have peritonitis despite NO abdominal symptoms other than a low grade fever.
So what is the STEP1 criteria for SBP? Paracentesis ASCITES FLUID PMN > 250, or a Positive Culture . Of course, you must also send it for total cell count, glucose, albumin,etc. You might get an oddball question about "milky" fluid in ascites. ANYTIME you have "milky" or "thick white" fluid in a CAVITY think Chylous or lymphatic rupture = triglycerides and/or lymphoma
What about bloody fluid? TB, TB, TB or CANCER, CANCER, CANCER
Thus, when should you perform a paracentesis in patients with ascites?
1) ALL first-time patients as diagnostic paracentesis to rule out SBP
2) ALL patients with new onset fever, leukocytosis, bandemia, left shift as diagnostic paracentesis for SBP
3) ALL patients who failed lifestyle modification + medical management as therapeutic paracentesis
3. Breaks stuff down: Ammonia (NH3) via AST/ALT into urea cycle.
So in cirrhosis, you have NH3 build-up leading to hepatic encephalopathy, which basically means A) "neurologically wasted", or everything slows down for patient B) asterixis "hand flapping" when elbows and wrists hyperextended. Exact mechanism has not been elucidated but for STEP1, know that
NH3 potentiates inhibitory neurons, aka GABAergic chloride channels = inhibition = slowing down.
NH3 inhibits excitatory neurons, aka Glutamatergic NMDA channels = inhibition = slowding down.
How do you treat this? Lactulose. Why in the world do you give an undigested sugar to treat hepatic encephalopathy? Because this is ingenious.
Basically, lactulose is like cellulose. Yes, it's NOT digested by our brush border enzymes and therefore reaches the colon intact. There, colonic gut bacteria ferment this sugar as well as All other undigested/unabsorbed sugars into Short Chain Fatty Acids (SCFA). And what do fatty acids have in common? Carboxylic Acid moiety which acidifies the colonic lumen. This then acidifies and ionizes NH3 (ammonia) into +NH4 (ammonium), thereby trapping the polar ionic ammonium within the gut lumen.
In summary,
A. lactulose indirectly acidifies and traps ammonia as polar less absorbable ammonium within the colon lumen for excretion.
B. Lactulose is 1st line treatment.
C. Rifaximin is 2nd line treatment. It is an antibiotic that targets NH3 (ammonia) producing colonic bacteria.
4. Breaks Stuff Down: toxins Hepatopulmonary syndrome
The exact mehanism is not fully understood, but in cirrhosis, a failing liver can't metabolize certain body toxins, some of which target pulmonary vasculature and cause a Nitric-Oxide mediated "global" pulmonary vasodilation. Why is this bad? When you dilate nearly ALL of your pulmonary vasculature, you worsen the physiologic Ventilation-Perfusion mismatch. Why? At rest, Not all of your alveoli and pulmonary vessels are open, but they matched up according to effects of gravity. (see diagram below). When you lie down, this gravity mediated V/Q mismatch is diminished.
Thus in hepatopulmonary syndrome, patients complain of dyspnea standing or sitting, which alleviates with lying down. A fancier term is called platypnea. Contrast this with orthopnea or dyspnea lying down in patients with heart failure, in which lying down causes more venous return to the heart, worsening pulmonary edema, which alleviates with sleeping at an angle. Hence the multiple pillows at night or in some severe CHF patients, they say, "doc, I've been sleeping on a recliner lately".
So STEP1 take-home for HPS: Worsening V-Q mismatch and increased A-a gradient secondary to NO-mediated vasodilation of pulmonary vasculature. This effect is WORSE standing up due to gravity, and gets better lying down = platypnea (dyspnea standing up, better in recumbent position). The only real treatment is? Get a new Liver = transplant.

5. Breaks stuff down: Hepatorenal syndrome
Same concept as hepatopulmonary syndrome. Diseased liver can't metabolize toxins, some of which target renal vasculature and instead of dilation, causes "global" renal vasoconstriction. Other factors include systemic vasodilation which triggers RAAS, ATIII and renal vasoconstriction. But bottom line:This puts kidneys in a chronic perfusion "starved" state and subsequent renal failure. So shitty GFR, Cr clearance, rising BUN:Cr ratio, etc. However, what defines hepatorenal syndrome is FAILURE of aggressive resuscitative fluids to recover renal function. Again, unlike normal acute kideny injury, whereby aggresive fluid administration can reverse the shitty GFR, Cr Clearance, these renal function labs do NOT recover when you give fluids in a patient with HRS. As in HPS, HRS can only be resolved with resolution of the failed liver = transplantation.
6. Abnormal blood flow
In a diseased liver, the splanchnic circulation (i.e. celiac, superior and inferior mesenteric venous plexi) DILATES and "sucks" all the blood from systemic circulation, thereby decreasing effective circulating intravascular volume. Thus a treatment principle hinges on reducing additional splanchnic vasodilation by giving a vasoconstrictor via
1) Non-selective beta-blocker: propranolol. Why non-selective? It does NOT selective for B1. So it's Both B1 and B2 antagonist. ***remember for STEP1 heart contractility, heart rate, conduction velocity = B1. Lungs, gut, uterus smooth muscle relaxation = B2. So bronchodilation = B2. Gut splanchnic vasodilation = B2. Uterus smooth muscle relaxation = B2. Thus, by blocking B2, you impede some of the unwanted splanchnic vasodilation and minimize further blood pooling into the gut, thereby improving the portal HTN. A side-effect, however with Non-selective beta blockers, is as you guessed it, bronchospasm.
2) Octreotide (somatostatin analog), similar principle as non-selective beta-blocker. It causes splanchnic vasoconstriction.
So how do you treat acute esophageal variceal bleed and achieve maintenance prophylaxis against future episodes?
Acute: Octreotide (medical) + sclerotherapy/electrocautery/balloon tamponade (surgical)
Prophylaxis: propranolol
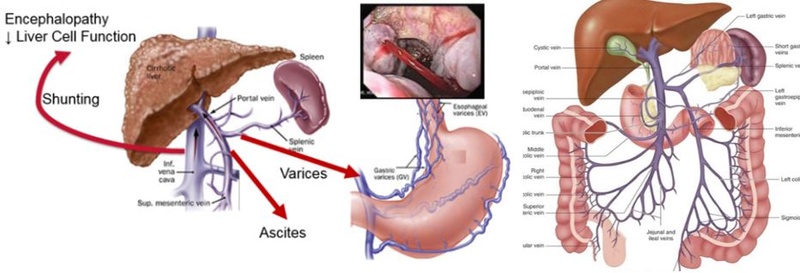
Portal System: Remember mainly all of your "Gut" organs drain first into your liver via the portal system: splenic vein, superior mesenteric vein, and inferior mesenteric vein.
You can get Portal Hypertension by any of the following methods
1) Within the liver: most commonly cirrhosis, less commonly: fibrosis, liver cancer, et.c
2) Outside the liver: portal vein thrombosis
3) Oustide the liver: Hepatic vein thrombosis (Budd-Chiari syndrome)
4) Outside the liver: Right heart failure which is most commonly caused by LHF --> RHF or Constrictive Cardiomyopathy, or anything that evenutally backs up to the right side of the heart and subsequently the liver. This causes a "nutmeg liver"
What happens in portal HTN? The dilated portal veins create new connections "anastamosis" with systemic system as a detour. Otherwise, the vein will keep on dilating and eventually burst.
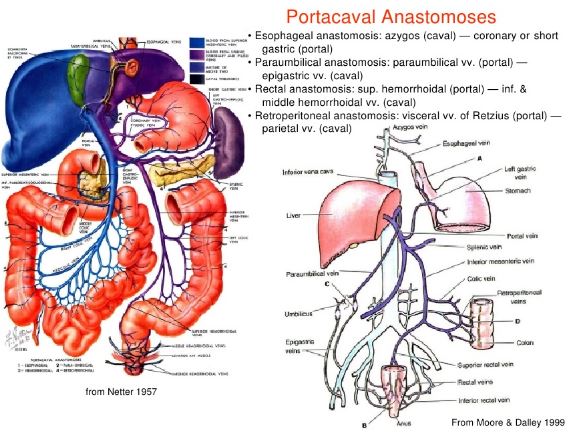
The STEP1 Take-home for Portal-Systemic Anastamosis are:
1. Esophageal: left gastric (portal) to esophageal vein (systemic)
2. Paraumbilical: paraumbilical vein (portal) to epigastric vein (systemic)
3. Rectal: superior hemorrhoidal/rectal vein to middle and inferior hemorrhoidal/rectal vein
Page 1 of 1
Permissions in this forum:
You cannot reply to topics in this forum